
| 22 October 2019
What is influenza?
Influenza (‘flu’) is an acute viral infection of the respiratory tract which spreads via air droplet secretions, aerosol or direct contact with respiratory secretions from an infected person. It’s very contagious, especially in closed communities such as residential care homes. Did you know, a single sneeze from an infected individual will project thousands of influenza viruses into the atmosphere?
Most causes of influenza in the UK occur during the colder winter months, so called ‘seasonal influenza.’ But the timing, extent and severity of this seasonal influenza can all vary from year to year.
Of course, coughs and colds are inevitable for most of us over the winter season, but if you ask anyone who has suffered from a bad bout of influenza, there is no comparison. For those who are normally fit and healthy, even though the unpleasant symptoms may pass in a week or so, the aftereffects of the flu virus can leave you tired and lethargic for some time after. Yet for those who are classed as vulnerable or high risk (e.g. the elderly, those with an underlying health condition and pregnant women) influenza can cause serious illness and sadly in some cases, death.
Short history
To date, the Spanish flu pandemic in 1918/19 remains the most lethal outbreak and until recently was arguably the most well-known. Fortunately, prevention and treatment has progressed in the last 100 odd-years but flu is still a serious threat on both a local and international level.
It’s 10 years now since the last pandemic of flu. In 2009 and 2010 the H1N1 virus (‘swine flu’) spread rapidly around the world; fortunately, the majority of UK cases were relatively mild, yet there were some serious cases. However, it’s not just a pandemic that can have a devastating impact.
Seasonal influenza can affect people from any age group. Illnesses range from mild (‘uncomplicated’) to severe and even death. Worldwide, annual flu outbreaks are estimated to result in approximately 3-5 million cases of severe illness and approximately 290,000 – 650,000 respiratory deaths.
In the UK, the reality is that every year, flu is a major factor in the ‘winter pressures’ that causes the NHS to come to a standstill – and comes with a heavy price tag. Yet, despite this, controversy and debate surrounding the only preventative method available continues.
The different strains
The World Health Organisation classes seasonal influenza as “an acute respiratory infection caused by influenza viruses which circulate in all parts of the world”. There are four types of the influenza virus: influenza A, B, C and D.
- Influenza A and B account for most infections.
- Influenza C virus is detected less frequently and as it usually causes mild infections it doesn’t present public health importance.
- Influenza D viruses usually affect cattle and aren’t known to infect humans.
The influenza A virus causes outbreaks most years and it is these viruses that are the usual causes of epidemics.
The influenza B virus tends to cause less severe disease and smaller outbreaks, although in children the severity of illness may be similar to that associated with influenza A.
As minor seasonal changes in the influenza virus occur it is important that the correct strains are included in annual vaccines. The World Health Organisation monitors global influenza epidemiology and advises on the composition of the forthcoming seasonal vaccines.
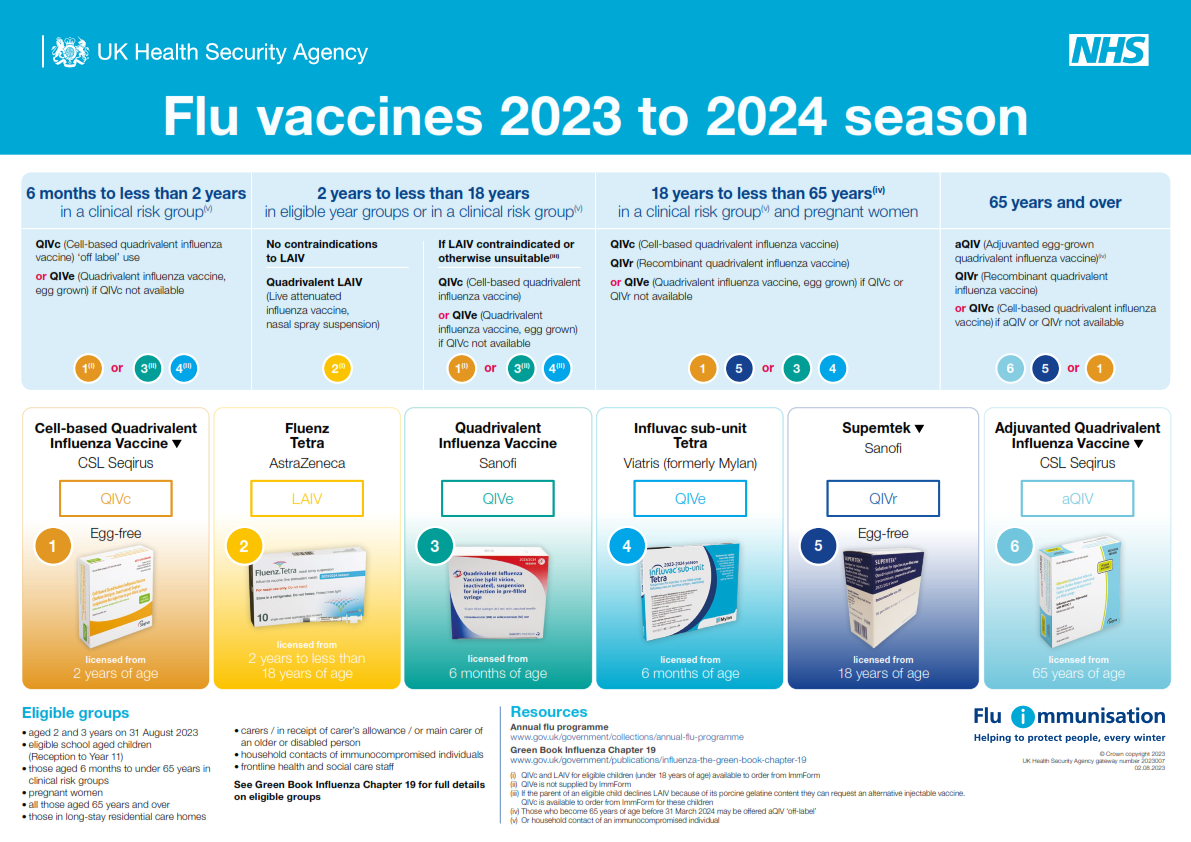
The image below shows the vaccines available for the 2023/2024 season.
Vaccination
On average, 8,000 people die from flu in England each year and some years the figure is much higher (e.g. according to Public Health England in 2017-18 there were an estimated 26,000 deaths were associated with ‘flu in England alone.) Therefore, vaccination is an essential preventative measure. And, as with all vaccines the principle of herd immunity applies: if enough people are vaccinated, it’s harder for the disease to spread.
In the UK the influenza vaccine is recommended for those who are most at risk of serious illness or death should they catch the infection. This includes:
- People over 65 years of age
- People aged 6 months to under 65 years in a clinical risk group, e.g.
- Chronic respiratory disease
- Chronic heart disease
- Chronic kidney disease
- Chronic liver disease
- Chronic neurological disease
- Adults with a Body Mass Index 40kg/m2
- People with diabetes
- People who are immunocompromised and adult household contacts of immunocompromised individuals
- Pregnant women aged 18 or over
- Frontline health and social care professionals
- Carers aged 18 or over
- Patients who are in nursing / care homes or other long-stay facilities
- Children aged 2 to 10 (but not 11 years or older): they receive the nasal spray vaccine
As most of you know, flu immunisation usually starts in September through into January the following year. Immunised individuals are generally protected within 14 days and protection lasts for at least one influenza season.
Moral debate
Since the pandemic of swine flu in 2009, most NHS frontline staff will be offered free vaccination as part of the annual flu campaign. The Government set a 90% flu vaccine target for health staff in 2019 – this is up considerably from reported uptake figures in frontline staff from the previous year (70% in England; 51% in Scotland, 56% in Wales and only 40% in Northern Ireland).
Yet even though some organisations robustly encourage staff to be vaccinated, there is no legal requirement for organisations to provide it or individuals to accept it. So, how do NHS trusts attempt to reach these ambitious targets? Some continue to rely on the goodwill of staff, whereas others are moving towards making the flu vaccine compulsory, similar to policies for Hep B.
In recent years several influential figures (including NHS England’s former medical director Sir Bruce Keogh and England’s former chief medical officer Dame Sally Davies) have voiced their public support for mandatory flu vaccination for staff. The arguments for compulsory vaccinations include increasing overall uptake (and herd immunity) as well as protecting patients, colleagues and their own families. However, reasons why some healthcare staff continue to refuse to be vaccinated include fears around effectiveness and possible side-effects. Others simply want a choice.
As you can imagine, intense debate surrounds the issue. The Royal College of Nursing (RCN), promote a culture of persuasion over compulsion. All nurses have a professional duty to protects their patients and the Nursing and Midwifery Council (NMC) code also states that nurses must ‘maintain the level of health needed to carry out your role’. However, the RCN’s professional lead for public health nursing, Helen Donovan believes that “if the vaccination was to become mandatory, rather than becoming a decision about what is right, it would become a decision on human rights and choices”. She’s also spoken out in favour of innovative ideas to increase the uptake, such as the London trust who gave a pound for each vaccination to a homelessness charity. Of this initiative Helen said, “that kind of action really speaks to nurses”.
Non-vaccine prevention
We know that influenza is highly contagious and is spread primarily through droplet infection or on contaminated hands. Therefore, promoting good respiratory and hand hygiene practices can help reduce the spread of the virus. The ‘Catch it, Bin it, Kill it’ campaign, initially introduced during the 2009 pandemic is still used to reinforce the importance of good respiratory and hand hygiene:
- Use disposable tissues to trap germs when you cough and / or sneeze: Catch it!
- Bin used tissues as quickly as possible: Bin it!
- Wash your hands often with warm water and soap: Kill it!
Remember too, there’s lots of self-care measures that you can implement and promote to keep healthy over the coming months. The NHS has lots of useful information and resources to help you and your patients stay well this winter.
Stay informed
There’s lots of ways you can keep up to date with what’s happening in the UK vaccination field, including:
- Subscribing to the Vaccine update newsletter
- Reading ‘Immunisation against infectious diseases: the Green Book’.
- Following Twitter hashtags such as #vaccineswork #flufighter
eLearning for healthcare
Unlock your potential – our healthcare eLearning courses make it simple to access high quality content, that deliver on your statutory and mandatory training and compliance needs.
