| 17 August 2023
What is the NHS Long Term Workforce Plan?
The newly launched NHS Long Term Workforce Plan, published June 2023, sets out the aspirations of the NHS to address existing and predicted workforce challenges. Over a 15 year period the aim is to train and retain thousands of staff – supported through reform to ways of working and training delivery (most notably through the introduction of a doctor apprenticeship).
The plan shows that, without concerted and immediate action, the NHS will face a workforce gap of more than 260,000-360,000 staff by 2036/37.
NHS Long Term Workforce Plan
It is a vital tool that NHS organisations of every shape and size can use over the coming years to define and address service level provision and understand the steps they can take to increase both the skills and capacity of the healthcare workforce.
The intention to train more frontline staff, whilst ramping up efforts to upskill and retain experienced staff, should help to alleviate some pressures on the service and will therefore be welcomed by patients and NHS organisations alike.
Jon Czul, Head of Consultancy and Research, Skills for Health
Six Steps Methodology to Integrated Workforce Planning®
Our Six Steps Methodology is the only one cited in the NHS Long Term Workforce Plan as a tool that Integrated Care Boards (ICBs) can use to help develop workforce plans. And that is exactly what Skills for Health have been helping the NHS do for many years – either through delivery of a Six Steps training programme (now CPD certified), or through direct help in researching, creating or auditing workforce plans.
The Six Steps Methodology identifies the elements that are needed in any workforce plan, taking into account the current and future demand for services, the local demographic situation, and the impact on other services – whilst helping you understand and work to a budget you can afford.
Our Six Steps Methodology is the only one cited in the NHS Long Term Workforce Plan as a tool that Integrated Care Boards (ICBs) can use to help develop workforce plans. And that is exactly what Skills for Health have been helping the NHS do for many years – either through delivery of a Six Steps training programme (now a certified training programme), or through direct help in researching, creating or auditing workforce plans.
The Six Steps Methodology identifies the elements that are needed in any workforce plan, taking into account the current and future demand for services, the local demographic situation, and the impact on other services – whilst helping you understand and work to a budget you can afford.
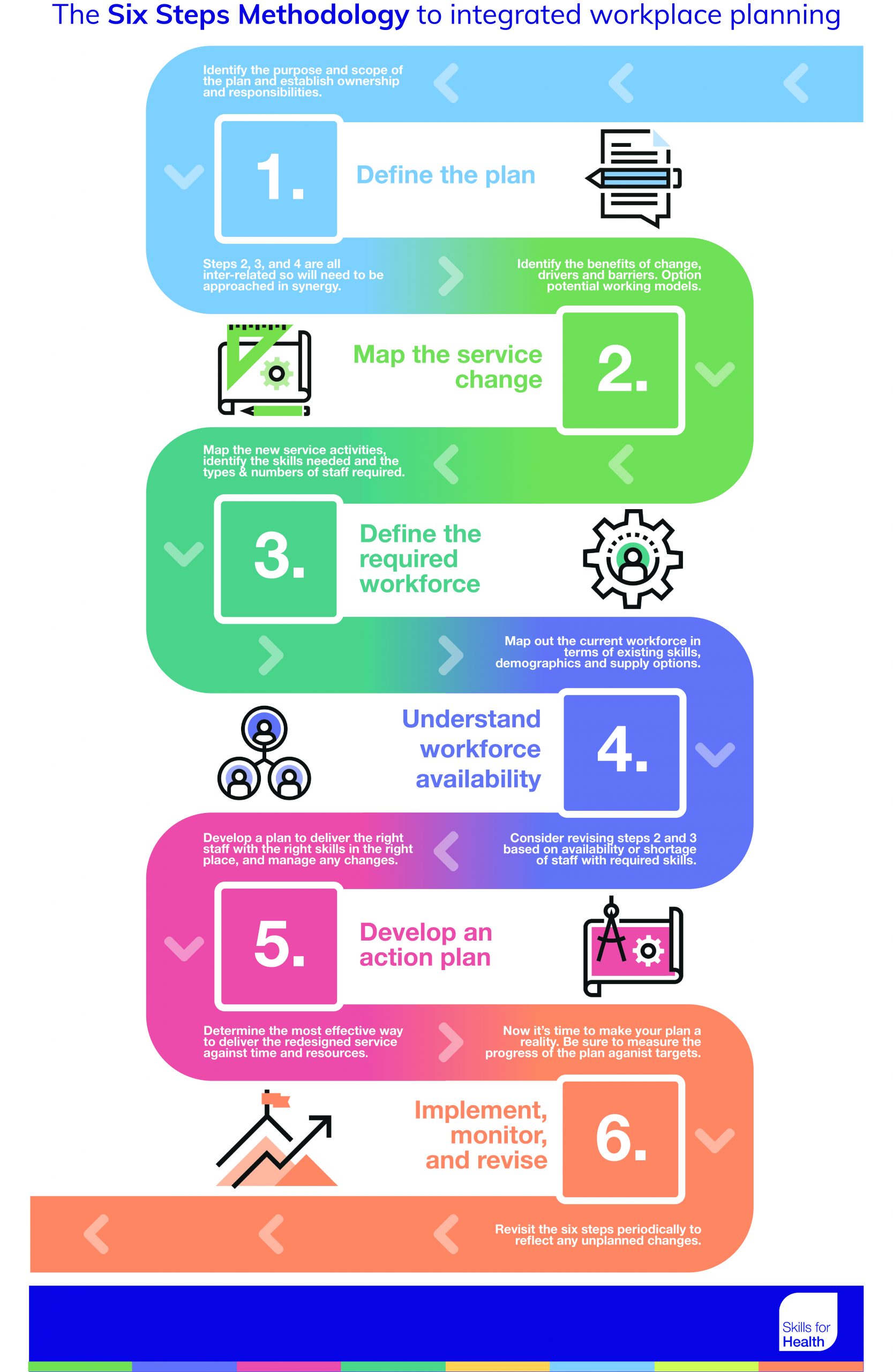
Skills for Health’s Six Step Methodology® builds into the process of workforce planning essential elements to ensure the quality of services are both discussed and planned for.
David Withers, Head of Education, Hull and East Yorkshire Hospitals NHS Trust
What are the actions NHS employers need to take?
As ever, the devil is in the detail and we echo the cautious optimism with which this plan is being greeted, recognising that whilst this is only a starting point, it at least sets out an ambition (if not a fixed roadmap) to begin to tackle the NHS’s workforce challenges.
Jon Czul, Head of Consultancy and Research, Skills for Health
The NHS Long Term Workforce Plan is a broad ambition. Skills for Health have been working with NHS providers for over 20 years to enhance and develop their workforce planning capabilities, so we asked our expert team to pull out some of the actions healthcare employers can take to translate ambition into reality.
The below list is by no means exhaustive, as the plan must be considered and adapted to many differing healthcare settings and requirements. We look forward to working with partners across the country to help identify and action the NHS’s staffing ambitions, and illuminating the implementation of the NHS Long Term Plan through our shared learning experiences.
Notes from the Long Term Plan
How to address and action
Apprenticeships
New apprenticeship pathways need to be developed and delivered, increasing to 22% of training for clinical staff up from current 7% by 2031, with a particular focus on Allied Health Professionals and podiatry
Aimed at employers and front-line managers, the Healthcare Apprenticeship Standards Online (HASO) is the best place to navigate apprenticeships and technical education in the health sector. Users can see and download all apprenticeship standards, and end point assessment plans; plan how to fund, procure, deliver and quality assure apprenticeships; find providers and end point assessment organisations; and create apprenticeship pathways for career progression.
It is the best place to find out about and join trailblazer groups that develop and deliver new apprenticeship standards.
Career and competence pathways
New roles need designing to meet the changing needs of patients and support the ongoing transformation of care.
Robust capabilities frameworks can help organisations understand the core skills and experiences that staff need to have. By providing a framework to match population health needs to service provision, they can greatly impact patient outcomes whilst supporting the development of individual staff.
Online learning
Online, digital and blended learning are key components of increasing accessibility of training. Organisations should look to develop their eLearning capabilities to support their workforce plans.
Increasing eLearning can help provide key skills in an easy, accessible way, reduce admin burden, and support individual development. Learning across organisations can be standardised and portable – for example by having courses aligned to the Core Skills Training Framework®, by using a Learning Management System (LMS), by being aligned to Career and Competence Frameworks, or by having blended learning leadership training programmes.
Workforce planning capability
The plan recommends actions at every level of the NHS – employers, systems and national organisations will all need to contribute. Increasing the capability of workforce planners across organisations and using a common language is vital to success
Increasing the capability of workforce planners across organisations and using a common language is vital to success. Using the Six Steps Methodology can enhance individual competency in workforce planning, and provide a consistent language and scope for organisations to collaborate and sync their workforce plans. Facilitated training programmes on Six Steps and workforce planning can help bring together and unify planners working towards common goals.
Leadership
Improving culture, leadership and wellbeing is a cornerstone of staff retention.
Leaders need to be well equipped to manage workforce development, ensure the provision of continuous learning and development, and create a culture where staff have access to the support and services they require. Activities like one-to-one coaching can help leaders progress and develop their capabilities to manage change and better serve the teams they support.
Understanding employee experience
The plan sets out a proposition that NHS organisations develop a clear employee value proposition (EVP) and promote this across the workforce.
To understand the unique value of a career in the NHS, organisations should look to understand their employee’s current experiences. This can help identify cultural drivers that need to be championed and developed, as well as pain points that need to be rectified as a part of retention efforts. Employee listening tools – like Ambit – should be used to ensure the workforce has a voice.
Understanding population trends
The workforce needs to be able to do more to prevent ill health, shifting from episodic to ongoing, chronic care – particularly for those wit multimorbidity, frailty and complex needs.
Undertaking research to understand health trends in local populations is key to understanding the service provision required by all organisations, from primary care to Trusts to Integrated Care Systems. These can then be mapped to competency frameworks to develop capacity and capability, and inform workforce plans at every level.
Identify skills gaps
Maintaining the current size of the workforce, and with skills mix within, will not be sufficient to deliver the care needed in the future.
Undertaking research, like a training needs analysis, can help organisations understand the skills and knowledge required by the workforce to meet service demands and developing population health trends. For example, Hampshire and Isle of Wight Integrated Care Board recently undertook research that helped them answer feedback that education, training and career development have not kept pace with the transformation in mental health service demands.
Planning at every level
The plan recommends actions at every level of the NHS – employers, systems and national organisations will all need to contribute.
Workforce planning should take place at multiple levels and in multiple different healthcare settings. These localised workforce plans can contribute to and be informed by an Integrated Care Systems workforce plan to deliver a robust programme of development and evidence how every part of the NHS is contributing to the Long Term Plan.
Expand enhanced, advanced and associate roles
Offering modernised careers with strong core skills, particularly that help with multimorbidity, frailty or mental health needs. Grow the workforce in these newer roles from 1% to 5%, with 6,300+ clinicians on advanced practice pathways by 2031.
Role design needs to be undertaken to provide new career pathways; based on identified skills and service gaps uncovered by research, and in line with population health trends.
Skills for Health have stood side by side with the NHS since 2002. We have supported the ever-changing landscape of healthcare across the UK, providing expert help where it is needed most. Our ambition is to help the NHS achieve a skilled, sustainable workforce that is ready to meet the challenges of today and the future.