| 5 August 2020
Whilst the majority of the world waits patiently for a vaccine to put an end to the death and economic destruction wrought by COVID-19, anti-vaxxers are joining anti-lockdown protests and using this time of uncertainty to spread misinformation and fear. Such an alliance is causing vaccine hesitancy to rise in the UK and across the world, posing a threat to public health. Here we will unpack everything about vaccines and the people they’re made for – from the science to the politics to the conspiracy theories they are entrenched in.
“Many aspects of modern life put us at more risk, however, we are more prepared (to face an outbreak) than ever before”
Despite being warned by scientists for years, ‘prepared’ is probably the last word you would use to describe the response to the current pandemic. The international race to obtain PPE, ventilators and, perhaps more than anything, space – for the dead and those struggling to live – are indicative of very little preparation or consideration for the threat coming our way.
“We’re only as secure in the world as the weakest country”
— Prof. Int Public Health, London School of Hygiene & Tropical Medicine
With the growing population, rising global travel and people living closer together in urban areas, the chance that an outbreak could have been controlled was reduced substantially because of the viruses’ incubation period.
Now the entire world has been brought to a standstill with governments struggling to safeguard public health through social distancing measures, and experts claiming that the only solution is a vaccine.
The aim of the vaccine? To attain herd immunity – that is, without millions dying. Herd immunity is when enough people in the population become immune to the virus that it no longer poses the threat of an outbreak. This can occur naturally or through a vaccination program. However, for us to attain herd immunity without a vaccine, 60-80% of the population would have to be infected. And, due to the virus’ high mortality rate, millions would have to die.
For this pertinent reason, a vaccine seems to be our final hope in surviving this pandemic.
Could it really get any worse?
The virus is believed to be more severe during the colder months and dry indoor air may encourage the spread of the disease.
In order to combat the expected spike in transmissions this flu season, Matt Hancock announced last week that over 30 million people will be administered a free flu jab in “The biggest flu-vaccination program in our country’s history”. That’s double the amount that were vaccinated last year – extended to those aged 50 to 64, individuals on the shielded patient list and members of their household, students in their first year of secondary school and all front-line health and social care workers.
Nevertheless, a well-known fact amongst legislative members and inherent in the ambitious nature of political vocations is what?
You cannot please everybody.
Despite the science, there is still a section of society that perceives vaccination to be the bigger threat than coronavirus.
Do vaccinations work?
Whilst the coronavirus is not the deadliest virus of the century, it has become the most widespread. The Spanish flu, Ebola Virus and SARS all showed us how deadly viruses can be. In fact, the very fact that coronavirus isn’t as lethal is the precise reason it is able to spread so quickly and extensively – most of its hosts live to transmit it to someone else, not to mention all the asymptomatic hosts that are spreading it unknowingly.
Vaccination is one of the best successes of modern medicine. In fact, immunization currently prevents 2-3 million deaths every year, with the WHO estimating at least 10 million deaths were prevented between 2010 and 2015 thanks to vaccinations delivered around the world. It safeguards people in all age groups from diseases like polio, tetanus, diphtheria, pertussis, measles, and whooping cough.
Because vaccination is cost-effective, it also promotes economic development and enables governments to focus on national priorities such as education and achieving the Sustainable Development Goals (SDGs). Since vaccination was introduced in the UK, diseases such as tetanus, polio and smallpox, which used to disable millions of people, have disappeared almost entirely. If vaccine administration is stopped, it could cause these diseases to reappear, as they have been doing recently. Cases of measles, for example, doubled from 2016 to 2018 and the occurrence of mumps rose from 573 cases in 2016 to 1061 in 2018.
Nevertheless, it’s impossible to know from even large clinical trials how vaccines will affect people with a range of different conditions; if vaccines will have adverse long-term effects; or what the impact of repeat doses might be if, as many expect, booster shots are required.
“Pretending science doesn’t contain uncertainty serves neither the scientists nor public health.”
— Therese Raphael, Bloomberg Opinion
While established vaccines have been linked to some rare cases of serious illness, researchers have not found a link between established vaccines and adverse impacts in most cases.
The Real Threat
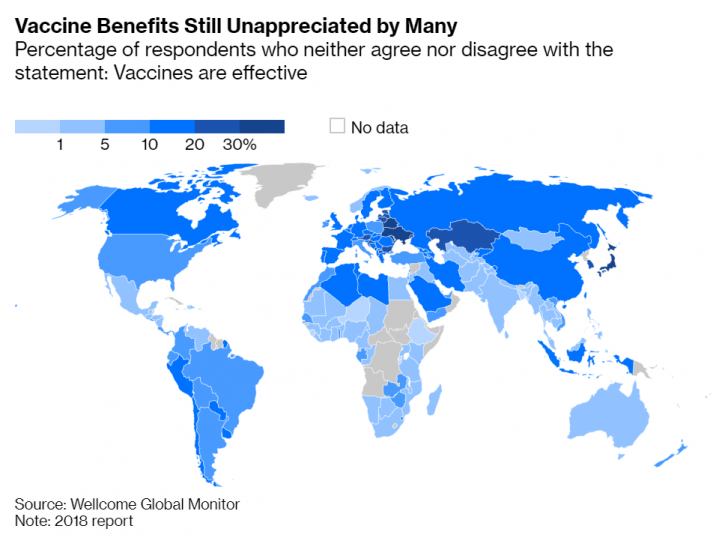
Globally, eight in ten people (79%) somewhat or strongly agree that vaccines are safe, while 7% somewhat or strongly disagree. Another 11% neither agree nor disagree, and 3% said they ‘don’t know’.
According to Dr. Anthony Fauci, the U.S.’s top infectious disease expert, even a vaccine that is 70% to 75% effective, if it is taken by only two-thirds of the public, it would not be successful enough in creating the herd immunity necessary for economies to get back up and running.
That is why the World Health Organization named vaccine hesitancy as one of the Top 10 Threats to Global Health in 2019.
Anti-vaccine rhetoric and growing suspicion of modern health practices among parents has led to a growth of vaccine hesitancy around the world.
One in six U.K. respondents to a YouGov survey taken in June said they definitely or probably would not get vaccinated. Meanwhile, a CNN poll showed a third of Americans would not try to get a vaccine if it existed.
Thus, governments have a lot riding on not only securing an immunization program but on making sure people take part.
Who are anti-vaxxers?
Vaccine hesitancy has been used to refer to people who hesitate, delay or refuse vaccinations, even when they are readily available.
The misled belief held is that vaccinations cause more harm than the virus itself. Such reasoning can be grounded in religious, philosophical or general mistrust of the pharmaceutical companies and/or doctors that administer, fund or make the vaccines.
Other’s beliefs are fed by a wider distrust of central government, associating vaccines with the establishment, political/coercive control and further-reaching conspiracy theories such as the current pandemic being a cover for a plan by Bill Gates to implant trackable microchips into people.
Although the rates of vaccine hesitancy in the UK are low, at 2% or less, the anti-vaccination hyperbole seems to be rising. Coverage rates for all 13 child-vaccinations fell last year in the UK and results from an ORB International survey carried out in early May found that 10% of respondents were unwilling to be vaccinated for COVID-19.
Jennifer Reich, a professor of sociology at the University of Colorado Denver, in her research on anti-vax parents, notes that healthcare decisions tend to be primarily a maternal decision. There is a generation of young mothers in the UK who are drawn to natural health remedies such as natural contraception and giving birth at home.
A clear understanding of what influences mothers and fathers to make such decisions is essential for healthcare practitioners, now more than ever, with the Coronavirus pandemic looming over our heads.
So why the hesitancy?
Recent research conducted by Valerie Haroune, a paediatric staff nurse at St Mary’s Hospital and Liz King, senior lecturer at Buckinghamshire New University, summarised the findings of 7 major pieces of research from the UK, US and Canada on parental vaccine hesitancy over the past decade.
Three major themes were identified in the study – parent’s beliefs on the safety of the vaccines, their views on vaccine effectiveness and their trust in healthcare providers.
1. Vaccine Safety
In all 7 of the studies, parent’s concerns about the safety of the ingredients in the vaccine were reported as the strongest factor guiding their vaccine hesitancy. Their fear regarding the toxicity of the vaccine – specifically about ingredients and side effects, including the risk of developing autism – outweighed any health outcomes associated with the vaccines.
A study conducted in Merseyside, England, on the refusal of parents to vaccinate following a measles outbreak found that their concerns over vaccinations’ link with autism was the largest factor in their refusal.
What’s baffling to many is that even though parents were aware of the harms of measles (the most serious complications including blindness, encephalitis, severe diarrhoea, ear infections and severe respiratory infections such as pneumonia), they still refused to vaccinate.
This could be a result of a cognitive pattern called the omission bias. The omission bias is our tendency to react more strongly to harmful actions than to harmful inactions. So if a parent vaccinates their child and he/she develops an illness, they will feel more guilty than if their child contracted the disease due to their refusal to vaccinate.
There are also doubts over the quality of a vaccine. One is the risk of fakes. The WHO says one in 10 medical products circulating in low and middle-income countries are falsified or do not meet standards. Falsified medicines lead to poisoning, untreated disease and other hazards. And COVID-related fraud, from masks to medicine, is booming, the United Nations has found. Vaccines will be a target, too. Officials have already discovered a fake Israeli coronavirus vaccine being sold in South America.
2. Effectiveness of Vaccines
Four out of the seven studies found that parents believed vaccines were no longer necessary for diseases that are now rarely seen.
This is reflected in the preliminary results of a survey carried out by the Vaccine Confidence Project and ORB International when infections in Europe were still rising rapidly in early April. They found vaccine resistance (as opposed to just hesitancy) to be especially high in countries that have managed to avoid the worst of the pandemic.
In Switzerland for example, where immunologists have proposed that mass vaccinations could take place as early as October, 20% of people said they would be unwilling to be vaccinated. In Austria, praised for their speedy flattening of the curve, vaccine scepticism was similarly rife, with 18% saying they would reject vaccination.
“Some of the scepticism reflects a mistrust of Big Pharma, some of it a mistrust of government. Some of it is simply because it’s been a long time since we lived in fear of the many diseases that vaccines now protect against.”
— Therese Raphael, Bloomberg Opinion
Another cause for the obsoleteness of vaccines was parents’ desire to treat their children with ‘natural immunity.’
Anti-vaccine mothers are especially concerned with the superiority of natural methods of immunisation over artificial vaccines. Many of them argue that having breastfed their children for more than two years has boosted their immune response, thus eliminating or greatly reducing the need for vaccinations.
Breastfeeding is well known to provide immune protection and prevent various diseases in the perinatal period, so does this argument have grounds?
Arguments in favour of the protective effect of breastfeeding include the “apparent capacity of breast milk factors to enhance maturation of the intestinal mucosal barrier and, thus, enhance the development of oral tolerance”. Unfortunately, the numerous confounding variables and potential for bias make definitive inferences very difficult.
There just isn’t enough evidence to show that breastfeeding protects against all illnesses in every case. And, to that end, it does not substantiate avoiding vaccination for your children. If anything, it only promotes the likelihood of your child reacting well to a vaccine (and thereby avoiding any of the side effects anti-vaxxers fear and use to justify their grounds).
3. Healthcare Factors
Alongside ideas about the ineffectiveness of vaccines, opinions on healthcare were equally as divisive – reported in four out of the seven articles in Haroune and King’s meta-analysis.
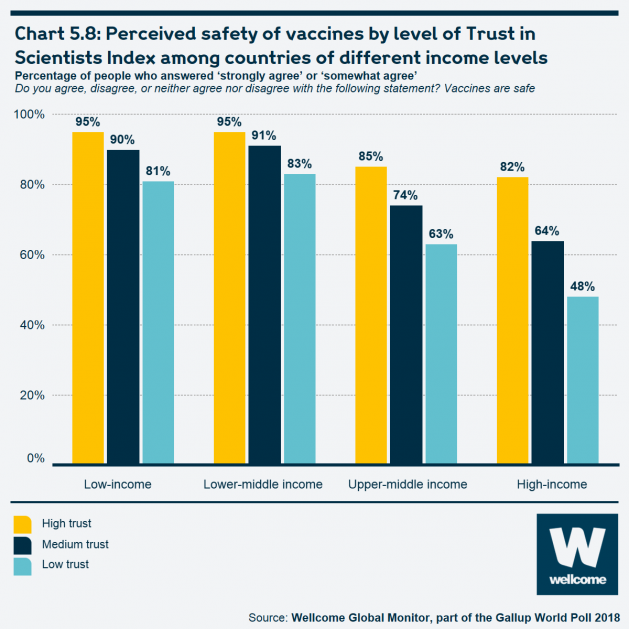
Distrust in pharmaceutical companies is strongly correlated with vaccine hesitancy and scepticism of science altogether. Comparably, according to the Wellcome Global Monitor:
- In most regions, people who have high trust in doctors and nurses are very likely to consider that vaccines are safe. However, this is less true in Western and Eastern Europ
- There is a clear positive relationship between overall trust in scientists, as measured by the Wellcome Trust in Scientists Index, and overall attitudes towards vaccines, though the relationship is strongest in high-income countries.
That trust was being sorely tested even before the pandemic. In the U.S., a near epidemic of overprescribing prescription medications, especially of opioids, has increased scepticism of both doctors and drug companies. Such scandals and pyramid schemes have cemented the idea in some that GPs and doctors are working alongside pharmaceutical companies to influence parents’ decisions in the pursuit of their own selfish interests.
Other parents have developed a distrust after having a negative interaction with a healthcare practitioner. Some women reported GPs to be ‘patronising’ and this was further exacerbated by parents’ perception that vaccine information found online was conflicting or not detailed.
Black and minority communities have been hit the hardest by Covid-19 and thus arguably have the most reason to line up for vaccines. Yet, vaccination rates are lower among minority groups due to lower levels of trust from historical abuses.
Barriers to successfully booking an appointment also caused delays in immunisation, with parents being too busy to book an appointment, or as in McHale’s study in the UK, children being too ill to be taken for an appointment.
Anti-Vaxxers vs COVID-19
Distrust of authorities has only got stronger in the last few months. During lockdown, thousands gathered in European cities to protest for the right not to be inoculated, as well as to vent their anger at “social distancing restrictions they believe to be a draconian ploy to suspend basic civil rights”.
In Germany, where protests have been rife, some believe the Covid-19 pandemic to be a hoax thought up by the pharmaceutical industry. This their apparent reasoning for acting against “enforced vaccinations”, despite health ministers favouring a voluntary programme, while the mooted introduction of ‘immunity passports’ was withdrawn from a new ‘pandemic law‘ passed through the Bundestag this month.
Natalie Grams, a doctor and author who specialises in debunking claims about the effectiveness of alternative medicine and who used to practise homoeopathy herself said the following:
“While there isn’t a vaccine but everyone is talking about one, the anti-vaccination movement has found a perfect environment to flourish. Whilst the big health bodies take weeks to formulate their messages, virologists are weighing up evidence and coming up with slightly conflicting advice. Anti-vaxxers are exploiting this uncertainty.”
— Natalie Grams
One hurdle for health-care authorities is convincing people that a vaccine produced at lightning speed is no less safe than one that would normally take more than a decade to develop.
Where does anti-vaccination come from and why is it so political?
Like everything else in the U.S., opinion on a vaccine varies along party lines, with 81% of Democrats and only 51% of Republicans keen to get vaccinated. In France (where one in three people disagree that vaccines are safe, the highest percentage for any country worldwide), anti-vaccination sentiments are seen as a phenomenon of the current millennium, fed by a wider distrust of central government. In German-speaking countries, by contrast, wariness of vaccination programmes dates back to the 19th century.
In the first half of the 20th century, anti-vaxxer views converged with anti-semitism: the Third Reich was rife with conspiracy theories presenting vaccination programmes as a Jewish plot to either poison the German nation or “submit humanity to Jewish mammonism”.
“There’s a real fear of an unholy alliance between esoteric leftwingers, the far-right and the Reichsbürger movement.”
— Natalie Grams
Anti-vaccination sentiment is usually at around 2-4% in Germany. But with this alliance, you are looking at broader resistance among the population.
Some historians believe that voluntary vaccination programmes against Covid-19 would not only be less politically risky but also more effective at protecting the population from coronavirus. However, if a vaccine over promises, if the risks are not clearly explained or if there are problems with delivery, it could further undermine trust in authorities, institutions and even experts, with far-reaching consequences for public health and the economy.
“It’s hard to imagine another time when there was so much riding not just on the science, but on how it’s communicated.”
— Therese Raphael
What can we do to help reduce vaccine hesitancy?
It is evident from this study that a lack of understanding of the crucial need for vaccination is the underlying factor in vaccine hesitancy worldwide.
- More than half the parents said that a discussion with a healthcare provider and transparent information would help them make a better decision.
- One-third of respondents claimed that easier access to a doctor would assist with vaccination.
If people are to have confidence in regulators’ declarations that a vaccine is “safe and effective,” much will depend on governments acknowledging their concerns and being transparent about both the benefits and the unknowns. All individuals will need to be provided with the most accurate, informative resources – standardised across the board so to avoid any conflicting information – empowering individuals to make the right choice for themselves, not made for them.
eLearning for healthcare
Unlock your potential – our healthcare eLearning courses make it simple to access high quality content, that deliver on your statutory and mandatory training and compliance needs.
